Integration of immersive virtual environments (IVEs) in healthcare research and design
This paper explores the integration of immersive virtual environments as a methodology in healthcare design research.
Introduction
Immersive virtual environments (IVEs)
The field of healthcare research and design is evolving with the adoption of innovative technologies, including virtual reality (VR), augmented reality (AR), and mixed reality (MR). These technologies enable researchers and practitioners to test environmental conditions and gather feedback in controlled, simulated settings.9,10 Among these technologies, immersive virtual environments (IVEs), a subset of VR, stand out from traditional 3D models owing to their heightened realism and user engagement.1-3
IVEs are advanced VR environments that engage multiple senses, including sight, sound, touch, and even smell, providing users with realistic and interactive experiences.11 These environments have become powerful tools in healthcare and environmental design research, offering multisensory, interactive simulations that closely replicate real-world settings.2 However, the fidelity of these virtual environments can vary, and they may not fully capture the complexity and richness of actual experiences, leading to potential discrepancies between virtual and real-life conditions.12 Typically accessed through VR headsets or CAVE (Computer Assisted Virtual Environment) systems that utilise large-scale projections, IVEs create immersive experiences of various environments.13
Numerous studies have demonstrated their effectiveness in promoting disability inclusion,9 enhancing multisensory engagement,11 providing methodological frameworks for environmental design,7 assessing seasonal variations in virtual nature experiences,14 and advancing nursing education programmes.8
Applications of IVEs in healthcare research and design
Integrating multi-sensory stimuli, IVEs significantly enhance users’ sense of presence, involvement, and realism, which are essential factors for effective training and research in healthcare settings.11,15 These computer-generated, three-dimensional environments rely on sophisticated hardware (such as haptic devices) and software (including real-time rendering engines) to create a psychological state in which users perceive the virtual setting as authentic.16,8 Over time, IVEs have developed into powerful tools that can simulate complex clinical environments, like surgical suites and paediatric patient rooms, with increasing precision and relevance to healthcare design.17,18
In healthcare design, immersive virtual environments are increasingly employed to evaluate and improve patient-centred settings. For example, Jiang et al.19 used IVE technology to examine how hospital greenspaces influence wayfinding and spatial experience. Their study found that visible greenery enhanced navigation and positively affected patients’ moods, illustrating the value of IVEs in guiding evidence-based design decisions that improve user experience.
Beyond environmental design, IVEs have demonstrated significant potential in clinical applications. In a controlled study, Maani et al.20 found that immersive virtual reality (IVR) significantly reduced pain intensity and discomfort during burn wound debridement in combat-injured soldiers, highlighting its relevance in acute care scenarios. IVEs have also been applied in healthcare education to improve training and assessment outcomes. Garrett et al.17 for instance, demonstrated that simulating home healthcare environments in VR enhances professional training and evaluative capabilities.
In broader educational contexts, IVEs have been shown to increase engagement and motivation. Peixoto et al.21 found that IVR technologies enhanced learner motivation and engagement in English as a Foreign Language (EFL) education, although they did not significantly outperform traditional methods in knowledge retention. Lin et al.,22 in a critical literature review, reported that the realism of VR environments positively influences learning across cognitive, behavioural, and affective domains. Similarly, Mao et al.23 found that immersive VR significantly improved procedural accuracy and learning outcomes in surgical training for healthcare students, further supporting the pedagogical value of IVEs. Recent research continues to confirm the broad effectiveness of VR-based learning. Studies by Goi,24 Kazu and Kuvvetli,25 and Suhag26 all reported improved student engagement and learning outcomes in higher education, highlighting the capacity of IVEs to bridge experimental rigor with real-world relevance across both design and educational applications.
IVEs in environmental design research
Beyond healthcare-specific applications, IVEs have proven useful in assessing environmental comfort and building performance. Heydarian et al.13 employed IVEs to analyse how design features and occupant choices impact lighting use in office spaces, revealing that user-controlled lighting systems can enhance energy efficiency and occupant satisfaction. In a more recent study, Arowoiya et al.27 conducted a pilot study using IVEs to compare thermal and visual comfort under varying activity levels, emphasising the need to consider occupant activity in environmental design. Collectively, these studies demonstrate the versatility of IVEs in improving design decisions, clinical practices, educational outcomes, and environmental comfort across various settings.
In addition to educational benefits, IVEs address critical research challenges, including ethical constraints when working with vulnerable populations, the high costs of physical prototyping, and the limitations of ecological validity in traditional research methods.4,7 By simulating interventions in controlled, low-risk environments, IVEs allow researchers to explore design solutions without exposing participants to harm. For instance, Abulawi28 engaged paediatric patients in virtual co-design workshops using IVEs, which helped reduce hospital-related stress and ensured ethical safety. Surgeons can also practice complex procedures in photorealistic VR simulations, decreasing operative risks and improving outcomes.29
Further highlighting the versatility of IVEs, Sedghikhanshir et al. (2024)12 conducted an empirical study examining the impact of green walls and their sizes on stress recovery and restoration within virtual office environments. By integrating IVEs with a climate chamber, the researchers maintained consistent thermal conditions while manipulating visual stimuli. The study found that while the presence of green walls contributed to stress reduction and restoration, the size of the green wall did not significantly influence these outcomes. These findings suggest that the restorative benefits of biophilic design elements may be more closely tied to their presence rather than their scale, offering valuable insights for designing restorative environments in settings with spatial limitations.
Advantages of IVEs for healthcare and environmental design research
The advantages of using IVEs for data collection in design research are significant. They allow participants to engage in realistic simulations that closely resemble actual conditions, providing more accurate assessments and feedback. Moreover, IVEs offer researchers a high degree of control over variables, facilitating systematic experimentation and enhancing reproducibility and ecological validity.30 This technology also supports rapid prototyping and real-time feedback, increasing both efficiency and flexibility in the design process. The evolution and application of IVEs in healthcare design and education signify a major shift toward more immersive, patient-centred approaches. By capitalising on advanced technologies to create realistic simulations, IVEs provide valuable tools for improving patient care, enhancing educational outcomes, and informing evidence-based design decisions in healthcare settings.
Abstract
Immersive virtual environments (IVEs) are advanced virtual reality (VR) environments that provide fully interactive, multisensory experiences, distinguishing themselves from traditional 3D models through heightened realism and engagement (Baritome, 2023). Their versatility makes them a transformative tool in healthcare research, addressing key challenges such as the ethical complexities of working with vulnerable populations, maintaining confidentiality and managing high implementation costs (Goncalves et al., 2012).
While VR has historically been employed as a distraction tool to alleviate pain and anxiety in medical settings (Richey et al., 2022), its standard applications often lack the immersive depth needed to replicate real-world conditions accurately (Rahim et al., 2024). IVEs, by contrast, immerse participants in lifelike, sensory-rich environments through a fusion of visual, auditory and tactile stimuli, enabling researchers to collect nuanced, real-time data (Smith, 2015; Joseph et al., 2020). This heightened level of realism makes IVEs particularly well suited for investigating the complex interplay between environmental design and patient wellbeing. By simulating real-world healthcare settings, IVEs also allow researchers to safely test interventions, optimise designs and explore patient-centric solutions in a controlled and cost-effective manner. Despite their potential, IVEs remain underutilised in healthcare design research (Joseph et al., 2020).
This research explores the integration of IVEs as a methodology in healthcare design research. A systematic literature review was conducted using Google Scholar and CINAHL Complete, focusing on empirical studies published since 2012 that employed IVEs in the context of healthcare and architectural design. Analysis identified several key applications for IVEs in healthcare settings, including:
1. navigation and spatial cognition research;
2. studying the relationship between the built environment and human behaviour;
3. design evaluations (pre-occupancy and post-occupancy);
4. supporting decision making in space planning, layout testing and perception studies;
5. testing environmental variables such as colour preferences, acoustics, lighting and window views.
By integrating IVE technology into the design process, researchers can adopt a scalable, patient-centred approach to evaluating and implementing design solutions in healthcare environments. This methodology bridges art, technology and architectural design, enabling more rigorous, empathetic and efficient explorations of healthcare spaces. IVEs represent a transformative opportunity to innovate healthcare design research, offering new pathways for enhancing patient outcomes and environmental efficacy.
Learning objectives
- Understand the role of IVEs in healthcare research
- Analyse applications of IVEs in design evaluation
- Evaluate the impact of IVEs on patient outcomes
Integrating multi-sensory stimuli, IVEs significantly enhance users’ sense of presence, involvement, and realism, which are essential factors for effective training and research in healthcare settings
Aim of the study
This paper will explore the integration of IVEs as a methodological approach in healthcare research and design, highlighting key applications in healthcare settings. It will demonstrate how incorporating this technology into the design process fosters a scalable, patient-centred approach to evaluating and implementing solutions. By bridging art, technology, and architectural design, IVEs support more rigorous, empathetic, and efficient explorations of the healthcare environment.
Objectives of the meta-analysis/meta-synthesis
The primary objectives of this meta-analysis/meta-synthesis are:
- to synthesise existing literature on Immersive Virtual Environments (IVEs) in healthcare, identifying key findings and trends that demonstrate their effectiveness and applicability; and
- to identify gaps in the current research and propose future directions to further enhance the utility and understanding of IVEs in healthcare contexts.
Methodology
Criteria for literature selection
Studies were selected based on their relevance to the application of IVEs in healthcare, including qualitative, quantitative, and mixed-methods approaches. The inclusion criteria focused on empirical studies published since 2012 that utilised IVEs in healthcare and architectural design contexts.
Search strategy and data extraction
A literature review was conducted to synthesise research on IVEs in healthcare and environmental design. The review utilised key databases, such as Google Scholar and CINAHL Complete, supplemented by hand searches and backward citation techniques. Relevant studies were identified using keywords such as “immersive virtual environments”, “healthcare”, “immersive virtual reality”, “VR in medical training”, and “healthcare design”. This comprehensive search strategy aimed to identify a wide range of studies, uncover research gaps, and highlight research gaps for future exploration, advancing our understanding of IVEs in healthcare design.
Findings
Application and efficacy of IVEs in healthcare research and design
The meta-analysis and synthesis of studies identified five core settings in which IVEs are applied in healthcare research and design, each demonstrating measurable impacts on clinical outcomes, cost efficiency, and user engagement. Analysis also identified several key evidence for IVE effectiveness applications and outcomes of IVEs in healthcare design research, as shown in Table 1.
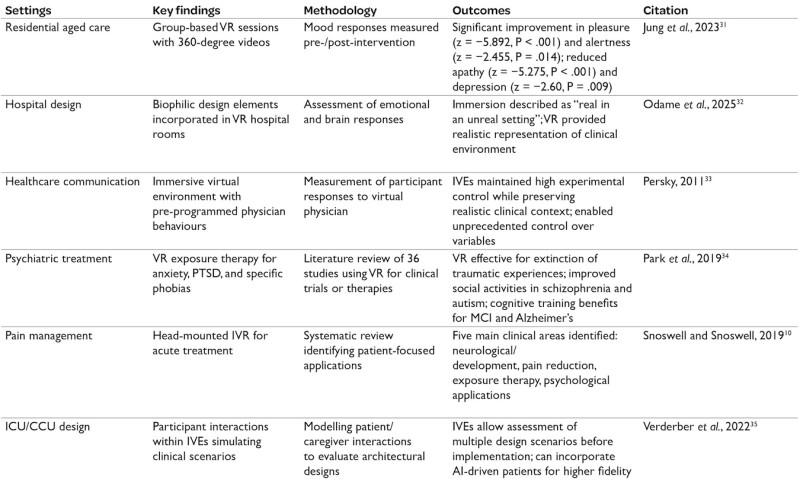 Table 1: Evidence for IVE effectiveness in healthcare applications and outcomes of IVEs in healthcare research
Table 1: Evidence for IVE effectiveness in healthcare applications and outcomes of IVEs in healthcare research
Applications of IVEs in healthcare and environmental design research
Navigation and spatial cognition research
Immersive virtual environments (IVEs) serve as valuable tools for studying navigation and spatial cognition. They provide controlled, immersive settings for investigating how users acquire spatial knowledge, navigate complex layouts, and develop cognitive maps of hospital environments. For instance, comparative studies between immersive VR and interactive map-based learning have shown that IVEs facilitate more naturalistic navigation and richer data collection, including eye and head movements, pointing tasks, and orientation measures.36 These capabilities allow researchers to analyse how users learn and recall spatial layouts, identify wayfinding issues, and evaluate the effectiveness of design elements, such as signage and landmarks, on navigation performance and user self-confidence.
Built environment and human behaviour
IVEs facilitate the exploration of how environmental factors such as spatial configuration, lighting, sound, and window views influence occupant behaviour, wellbeing and performance.37,35 By isolating and manipulating variables within virtual environments, researchers can track real-time behavioural responses (e.g., movement patterns, task completion), assess subjective experiences, such as comfort, satisfaction, and perceived safety, and obtain physiological measures like stress levels during navigation tasks.37
Design evaluations: Pre-occupancy
IVEs enable stakeholders to preview and assess planned healthcare spaces before construction. For instance, VR mock-ups of medication rooms have been utilised to simulate workflows, identify design flaws, and gather user feedback, leading to design improvements that enhance quality and patient safety.38,39 The primary advantages of using IVEs for pre-occupancy evaluation include cost-effectiveness, as they allow for repeated testing of multiple design options without the financial and logistical burdens associated with physical mock-ups. Additionally, they facilitate realistic simulations of staff and patient interactions, providing valuable insights into workflow dynamics. Furthermore, IVEs support the early identification of potential bottlenecks or risk factors based on user data, guiding timely and informed design adjustments.
Design evaluations: Post-occupancy
After a facility is in use, IVEs can replicate its real-world conditions to measure user satisfaction, workflow efficiency, and the outcomes of design changes. These simulations can facilitate continuous improvement by enabling the comparison of pre- and post-occupancy user experiences and the evaluation of design interventions based on real outcomes.38, 39
Facilitating decision-making in space planning and perception studies
IVEs enhance collaboration among architects, clinicians, and patients by enabling users to visualise and refine healthcare spaces in real time. They support decision-making by allowing users to test different arrangements of furniture, equipment placement, and room layouts dynamically. In addition, IVEs facilitate perception studies in which users assess comfort, convenience, and satisfaction when exposed to varying environmental conditions, such as illumination, noise levels, and colour schemes.37,35 These environments also enable the collection of both objective data, such as movement patterns, collisions, and heatmaps, and subjective feedback gathered through questionnaires and interviews, which together inform evidence-based design decisions.39.35
Testing environmental variables
IVEs offer the ability to manipulate environmental parameters with precision.35 For example:
- Colour preferences: Users can evaluate different colour schemes for walls, furnishings, and artwork, isolating their effects on mood and satisfaction.35
- Acoustics: Ambient and directional noises can be layered to examine the impact of noise on stress, communication, and task performance.35
- Lighting: Simulation lighting allows the measurement of natural vs. artificial illumination, circadian impact, and user preference.35
- Window views: Virtual windows may display varying views (nature, cityscape, abstract art) to examine effects on wellbeing and subjective comfort.40,37
User experience outcomes
Research utilising IVEs in healthcare settings has yielded measurable benefits. For instance:
- Comfort and satisfaction: Participants report higher perceived comfort and satisfaction when able to interactively evaluate and influence design elements.37,39
- Convenience and productivity: Workflow simulations reveal design elements that optimise staff efficiencies and reduce errors.38,35
- Health and wellbeing: Controlled studies show that environmental manipulations in IVEs can reduce stress, enhance mood, and support cognitive and physical rehabilitation.37
- Safety: Collision tracking and heatmaps identify potential hazards, enabling safer spatial organisation.35
- Social engagement and communication: IVEs support studies of team dynamics, patient-family interactions, and the influence of design on social connection).35

Discussion
Immersive Virtual Environments are playing an increasingly vital role in healthcare research and design. The reviewed literature highlights IVEs’ potential to address longstanding challenges in the field, including ethical concerns, high implementation costs, and the need for realistic, patient-centred research methods. By delivering fully interactive, multisensory simulations, IVEs surpass traditional 3D models and basic virtual reality applications, enabling researchers to recreate healthcare settings with high fidelity and experimental control.
The findings indicate that IVEs are being utilised primarily in five key areas: navigation and spatial cognition research; studies on the built environment and human behaviour; pre- and post-occupancy design evaluation; space planning and decision support; and environmental variable testing (e.g., lighting, acoustics, and window views). In each of these domains, IVEs facilitate more realistic and nuanced data collection by allowing for the assessment of user navigation, behavioural responses, physiological indicators, and subjective experiences.
For instance, studies cited in this review demonstrate that IVEs can effectively show the impact of design interventions on wayfinding, stress reduction, and user satisfaction – providing valuable insights for healthcare architects and planners. Moreover, the integration of IVEs into healthcare education and clinical training has been shown to enhance learning outcomes, increase learner motivation, and improve the realism of simulation-based environments. Empirical evidence supports their use in nursing education, procedural training, and co-design with vulnerable populations – contexts in which ethical and logistical constraints often limit the feasibility of traditional research methods. Importantly, IVEs enable rapid prototyping and real-time feedback, making the design process more adaptable and efficient without sacrificing ecological validity.
Despite these strengths, this review also identifies several limitations and gaps in the literature. While IVEs can simulate real-world scenarios with considerable accuracy, concerns persist regarding the fidelity of these simulations and whether they can fully replicate the complexity and richness of real-life experiences.
Conclusion
This meta-synthesis and analysis of current empirical work confirm that immersive virtual environments represent a significant methodological advancement in healthcare research and design. IVEs enable researchers and practitioners to conduct systematic, patient-centred studies in controlled yet realistic settings, thereby avoiding many of the ethical, logistical, and financial constraints associated with traditional approaches. Their versatility is evident in applications ranging from spatial cognition and behavioural studies to clinical training and participatory design.
To fully capitalise on the potential of IVEs, future research must address the enhancement of simulation realism and usability, investigate the long-term impacts of IVE-based interventions, and develop standardised protocols for their application in healthcare design and assessment. Bridging these gaps will make IVEs more applicable and facilitate the translation of emerging virtual methodologies into demonstrably improved patient care. This progress is likely to result in more satisfied healthcare workers and a more structured, responsive care environment.
In conclusion, IVEs serve as a critical bridge between evidence-based healthcare design and emerging technology, opening new avenues for compassionate, effective, and impactful research. As technology continues to evolve and gain broader acceptance, IVEs are poised to become an essential tool in advancing both the art and science of healthcare research and design.
About the authors
Michelle Pearson PhD is associate professor, Department of Design, at Texas Tech University.
Nishan Khatiwada MS, BArch, LEED Green Associate is a doctoral student, Department of Design, at Texas Tech University.
Daphne A. U. Chilaka MSc, MS, WELL AP, LEED Green Associate is a doctoral student, Department of Design, at Texas Tech University.
Farzane Omidi MArch, MS, EDAC, LEED Green Associate is a doctoral candidate, Department of Design, at Texas Tech University.
References
- Baktash, H, Kim, D, and Shirazi, A. (2024). Beyond sight: Comparing traditional virtual reality and immersive multisensory environments in stress reduction of university students. Frontiers in Virtual Reality, 5, 1412297. https://doi.org/10.3389/frvir.2024.1412297
- Lyu, K, Brambilla, A, Globa, A, and de Dear, R. (2023). An immersive multisensory virtual reality approach to the study of human-built environment interactions. Automation in Construction, 150, 104836. https://doi.org/10.1016/j.autcon.2023.104836
- Shaw, E, Roper, T, Nilsson, T, Lawson, G, Cobb, S V G, and Miller, D. (2019). The heat is on: Exploring user behaviour in a multisensory virtual environment for fire evacuation. Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems (pp. 1-13). https://doi.org/10.1145/3290605.3300856
- Gonçalves, R, Pedrozo, A L, Coutinho, E S F, Figueira, I, and Ventura, P. (2012). Efficacy of virtual reality exposure therapy in the treatment of PTSD: A systematic review. PloS One, 7(12), e48469–e48469. https://doi.org/10.1371/journal.pone.0048469
- Richey, A E, Hastings, K G, Karius, A, Segovia, N A, Caruso, T J, Frick, S, and Rodriguez, S. (2022). Virtual reality reduces fear and anxiety during pediatric orthopaedic cast room procedures: A randomized controlled trial. Journal of Pediatric Orthopaedics, 42(6), e634–e640. https://doi.org/10.1097/BPO.0000000000002250
- Rahim, N A A, Norasikin, M A, and Maksom, Z. (2024). 5 scientific problems for immersive interactions design within virtual reality applications development pipeline. Journal of Theoretical and Applied Information Technology, 102(20).
- Joseph, A, Browning, M H E M, and Jiang, S. (2020). Using immersive virtual environments (IVEs) to conduct environmental design research: A primer and decision framework. HERD: Health Environments Research & Design Journal, 13(3), 11–25. https://doi.org/10.1177/1937586720924787
- Smith, J W. (2015). Immersive virtual environment technology to supplement environmental perception, preference and behavior research: A review with applications. International Journal of Environmental Research and Public Health, 12(9), 11486–11505. https://doi.org/10.3390/ijerph120911486
- Goncalves, G, Monteiro, P, Coelho, H, Melo, M, and Bessa, M. (2021). Systematic review on realism research methodologies on immersive virtual, augmented, and mixed realities. IEEE Access, 9, 89150–89161. https://doi.org/10.1109/ACCESS.2021.3089946
- Snoswell, A J, and Snoswell, C L. (2019). Immersive virtual reality in health care: Systematic review of technology and disease states. JMIR Biomedical Engineering, 4(1), e15025. https://doi.org/10.2196/15025
- Gonçalves, G, Peixoto, B, Melo, M, and Bessa, M. (2025). Theoretical model validation of the multisensory role on subjective realism, presence and involvement in immersive virtual reality. Computer Graphics Forum. https://doi.org/10.1111/cgf.70145
- Sedghikhanshir, A, Zhu, Y, Beck, M R, and Jafari, A. (2024). Exploring the impact of green wall and its size on restoration effect and stress recovery using immersive virtual environments. Building and Environment, 262, 111844. https://doi.org/10.1016/j.buildenv.2024.111844
- Heydarian, A, Carneiro, J P, Gerber, D, Becerik-Gerber, B, Hayes, T, and Wood, W. (2015). Immersive virtual environments versus physical built environments: A benchmarking study for building design and user-built environment explorations. Automation in Construction, 54, 116–126. https://doi.org/10.1016/j.autcon.2015.03.020
- Litleskare, S, and Calogiuri, G. (2023). Seasonal variations in the effectiveness of immersive virtual nature. HERD: Health Environments Research & Design Journal, 16(1), 219-232. https://doi.org/10.1177/19375867221127420
- Miller, H L, and Bugnariu, N L. (2016). Level of immersion in virtual environments impacts the ability to assess and teach social skills in autism spectrum disorder. Cyberpsychology, Behavior, and Social Networking, 19(4), 246-256. https://doi.org/10.1089/cyber.2014.0682
- Kalantari, S, and Neo, J R J. (2020). Virtual environments for design research: Lessons learned from use of fully immersive virtual reality in interior design research. Journal of Interior Design, 45(3), 27–42. https://doi.org/10.1111/joid.12171
- Garrett, B, Taverner, T, Gromala, D, Tao, G, Cordingley, E, and Sun, C. (2018). Virtual reality clinical research: Promises and challenges. JMIR Serious Games, 6(4). https://doi.org/10.2196/10839
- Heydarian, A, Carneiro, J P, Gerber, D, Becerik-Gerber, B, Hayes, T, and Wood, W. (2015). Immersive virtual environments versus physical built environments: A benchmarking study for building design and user-built environment explorations. Automation in Construction, 54, 116–126. https://doi.org/10.1016/j.autcon.2015.03.020
- Jiang, S, Allison, D, and Duchowski, A T. (2022). Hospital greenspaces and the impacts on wayfinding and spatial experience: An explorative experiment through immersive virtual environment (live) techniques. HERD: Health Environments Research & Design Journal, 15(3), 206–228. https://doi.org/10.1177/19375867211067539
- Maani, C V Hoffman, H G, Morrow, M, Maiers, A, Gaylord, K, McGhee, L L, and DeSocio, P A. (2011). Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like, arm-mounted VR goggles. The Journal of Trauma, 71(1 Suppl), S125–S130. https://doi.org/10.1097/TA.0b013e31822192e2
- Peixoto, B, Bessa, L P, Goncalves, G, Bessa, M, and Melo, M. (2023). Teaching EFL with immersive virtual reality technologies: A comparison with the conventional listening method. IEEE Access, 11, 1–1. https://doi.org/10.1109/ACCESS.2023.3249578
- Lin, X P, Li, B B, Yao, Z N, Yang, Z, and Zhang, M. (2024). The impact of virtual reality on student engagement in the classroom – a critical review of the literature. Frontiers in Psychology, 15, 1360574–1360574. https://doi.org/10.3389/fpsyg.2024.1360574
- Mao, R Q, Lan, L, Kay, J, Lohre, R, Ayeni, O R, Goel, D P, and SA, D de. (2021). Immersive virtual reality for surgical training: A systematic review. The Journal of Surgical Research, 268, 40–58. https://doi.org/10.1016/j.jss.2021.06.045
- Goi, C L. (2024). The impact of VR-based learning on student engagement and learning outcomes in higher education. H K Noor and M A Rahman (Eds.), Teaching and learning for a sustainable future (pp. 207–223). IGI Global. https://doi.org/10.4018/978-1-6684-9859-0.ch012
- Kazu, İ Y, and Kuvvetli, M. (2023). The impact of virtual reality technology on student engagement and learning outcomes in higher education. Paper presented at the 2nd International Conference on Recent Academic Studies (ICRAS 2023), Konya, Türkiye. Retrieved May 27, 2025, from http://bit.ly/4r34mY7
- Suhag, N. (2024). The impact of virtual reality on student engagement in higher education. SSRN. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=5016008
- Arowoiya, V A, Moehler, R C, Fang, Y, and Poulami Jha. (2025). Comparative assessment of thermal and visual comfort in immersive virtual environments based on varied activity intensity: A pilot experimental study. Indoor Air, 2025(1). https://doi.org/10.1155/ina/2258335
- Abulawi, R A. (2023). The conceptual design themes of artwork in the public spaces of children’s hospital. Civil Engineering and Architecture, 11(5), 2413-2434. https://doi.org/10.13189/cea.2023.110513
- Wang, L. (2023). Application of virtual reality technology in environmental art design. Lecture Notes of the Institute for Computer Sciences, Social-Informatics and Telecommunications Engineering, 466, 591–601. https://doi.org/10.1007/978-3-031-23947-2_62
- Pan, X, and Hamilton, A F. (2018). Why and how to use virtual reality to study human social interaction: The challenges of exploring a new research landscape. British Journal of Psychology, 109(3), 395–417. https://doi.org/10.1111/bjop.12290
- Jung, D, Kim, D I, and Kim, N. (2023). Bringing nature into hospital architecture: Machine learning-based EEG analysis of the biophilia effect in virtual reality. Journal of Environmental Psychology, 89, 102033. https://doi.org/10.1016/j.jenvp.2023.102033
- Odame-Amoabeng, S, Akalin, A, D’haenens, F, Tricas-Sauras, S, and Chang, Y-S. (2025). Immersive insights: A qualitative systematic review and thematic synthesis of views, experiences, health and wellbeing of students and educators using virtual reality in nursing and midwifery education. Nurse Education Today, 150, 106679. https://doi.org/10.1016/j.nedt.2025.106679
- Persky, S. (2011). Employing immersive virtual environments for innovative experiments in health care communication. Patient Education and Counseling, 82(3), 313–317. https://doi.org/10.1016/j.pec.2010.12.007
- Park, M J, Kim, D J, Lee, U, Na, E J, and Jeon, H J. (2019). A literature overview of virtual reality (VR) in treatment of psychiatric disorders: Recent advances and limitations. Frontiers in Psychiatry, 10. https://doi.org/10.3389/fpsyt.2019.00505
- Verderber, S, Parshuram, C, and Gray, S. (2022, June). Creating, testing and evaluating immersive virtual ICU-CCU built environments. European Healthcare Design Conference 2022, London, UK. Centre for Design + Health Innovation, University of Toronto. https://www.daniels.utoronto.ca/sites/default/files/2023-06/EHD_VR%206_22.pdf
- König, S U, Keshava, A, Clay, V, Rittershofer, K, Kuske, N, and König, P. (2021). Embodied spatial knowledge acquisition in immersive virtual reality: comparison to map exploration. Frontiers in Virtual Reality, 2. https://doi.org/10.3389/frvir.2021.625548
- Altaf, B, Tavakoli, A, Bianchi, E, Landay, J, and Billington, S L. (2024). Leveraging immersive virtual environments for occupant wellbeing analysis. Computing in Civil Engineering 2023, 85–92. https://doi.org/10.1061/9780784485248.011
- Shultz, J, and Jha, R. (2021). Using virtual reality (VR) mock-ups for evidence-based healthcare facility design decisions. International Journal of Environmental Research and Public Health, 18(21), 11250. https://doi.org/10.3390/ijerph182111250
- Mastrolembo Ventura, S, Castronovo, F, and Ciribini, A L C. (2020). A design review session protocol for the implementation of immersive virtual reality in usability-focused analysis. Journal of Information Technology in Construction, 25, 233–253. https://doi.org/10.36680/j.itcon.2020.014
- Pearson, M, Gaines, K, Pati, D, Colwell, M, Motheral, L, and Adams, N G. (2019). The physiological impact of window murals on pediatric patients. HERD: Health Environments Research & Design Journal, 12(2), 116-129. https://doi.org/10.1177/1937586718800483
Presenters

Event news
Thinking on a new hospital – our keys for Pisa, hospital of the future
3rd November 2025
The benefits of joining up mental and physical health services
3rd November 2025
Contributing to a decade of transformation in healthcare
3rd November 2025